Retinal Lasers
Lasers are specialised narrow beams of light that have the ability to precisely focus on the target area. Due to the precise control they offer in the hands of the surgeon, they have been used for various purposes in medicine, especially in Ophthalmology.
There are various types of lasers and each laser has a different role to play in the treatment of eye diseases like cataract, glaucoma, retina, etc. In retina, mainly the Green lasers or the Red lasers are used. Depending on the purpose for which they are used in various retinal diseases. Laser procudures are not surgeries and are carried out in the out patient department only. After adequate dilatation, the patient is asked to sit or lie down (depending on the type of laser) and anesthetic drops are put in the eye. Laser shots are given at repeated intervals till the treatment is complete. There is usually no or mild pain. On occasion though some sensitive eyes could feel a stinging sensation in the eye or the head that is monmentary only.
There are no precautions to be taken either before or after the laser treatment.
Multiple such sittings may be needed based on the disease condition.
Pan Retinal Photocoagulation (PRP) laser: Diabetic Retinopathy, Retinal Venous Occlusions, Vasculitis, etc.
Barrage laser: Retinal degenerations, Retinal holes, Sub-clinical Retinal Detachments
Grid and Focal Laser: Diabetic Maculopathy
Photodynamic Therapy (PDT): Age-Related macular Degeneration, Idiopathic Polypoidal Choroidal Vasculopathy (IPCV)
ROP Lasers: Retinopathy of Prematurity
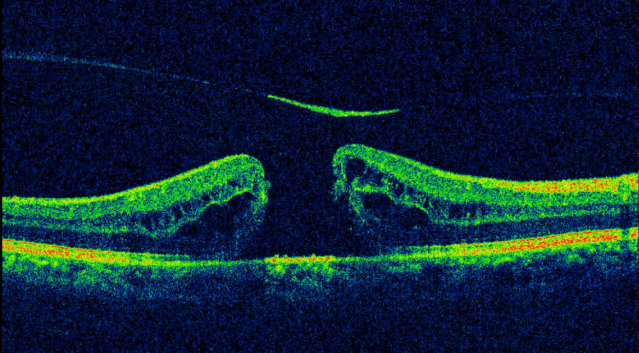
Central Serous Chorioretinopathy (CSCR /CSR)
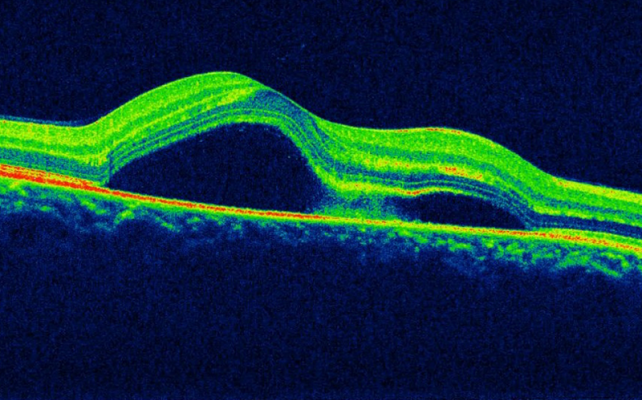
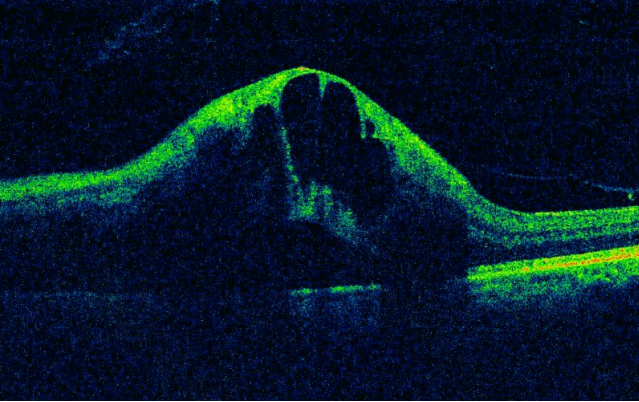
In Central serous chorioretinopathy (CSCR), fluid accumulates under the
macula causing a swelling.
Normally there is an RPE (retinal pigment epithelial) pump in the retina that
prevents any fluid from accumulating. When the RPE pump does not work as
it should, fluid builds up under the RPE. As a result, a small elevation forms
under the retina, causing vision to become distorted.
CSCR usually affects one eye at a time.
Patients usually complain of distorted, dull or blurred vision. Some may see a dark round patch in the central vision and objects appear smaller or further away than they are.
Risk factors include:
- 30-50 year old Males
- Stress
- Sleep disturbances
- Smoking or tobacco intake
- Use of steroids in any form
- Type A behavior (aggressive and competitive behavior)
- High blood pressure
A retina specialist can diagnose CSCR just by examination. An OCT scan will tell the amount of fluid under the macula and decide the further course of action. A fluorescein angiography (FFA) identifies the point of leakage in case treatment is planned.
Most cases clear up in one or two months without any treatment. However if there is severe vision loss or the fluid does not go away, then laser treatment may be used. These treatments can seal the leak and restore vision.
In some cases, vision may not be as good as it was before the condition. About half of the patients are at risk of having it again. It is important to have regular follow-up exams because long-term fluid accumulation can lead to permanent vision loss.

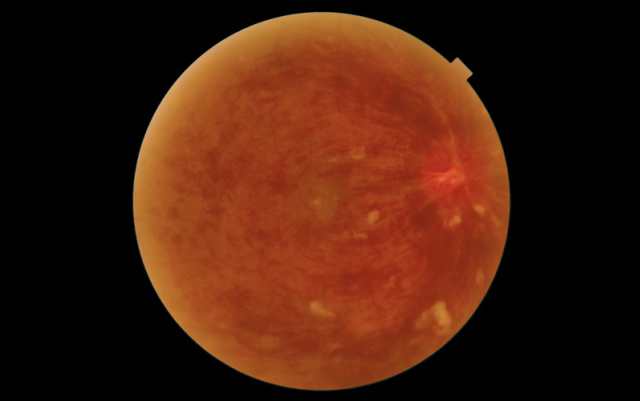
Retinal Vein Occlusions (BRVO, CRVO)
The retina has one main artery and one main vein to carry blood to and fro. When the main retinal vein becomes blocked, it is called central retinal vein occlusion (CRVO). When branches (tributaries) of the retinal vein become blocked, it is called branch retinal vein occlusion (BRVO).
When the vein is blocked, blood and fluid spills out into the retina. The macula can swell from this fluid, affecting the central vision. Without blood circulation, nerve cells in the eye can die and more vision could be lost. At times body creates new blood vessels (neovascularisation) to compensate for the block. However these are fragile and create more problems. In BRVO these are usually found on the retina (NVE) or the disc (NVD) and can lead to bleeding in the vitreous. In CRVO they are formed on the iris (NVI) in front part of the eye causing eye pressures to rise (glaucoma).
Most patients present with blurry vision that happens suddenly or over several days. If bleeding occurs, it causes floaters or a sudden drop in vision. Glaucoma causes pain and pressure in the affected eye.
RVOs almost always happen in one eye at a time. RVO usually happens in people who are aged 50 and older. People with high blood pressure, diabetes, glaucoma and hardening of the arteries (called arteriosclerosis) are at a higher risk.
To lower your risk for BRVO, you should do the following:
- Eat a low-fat diet
- Get regular exercise
- Maintain an ideal weight
- Avoid smoking and tobacco
A retina specialist can diagnose an RVO by examination. An OCT scan will tell the amount of swelling on the macula and decide the treatment. A fluorescein angiography identifies the blocked vessels and also the abnormal new vessels.
Since BRVO cannot be cured, the main goal of treatment is to keep the vision stable. Swelling of the macula is best treated with intravitreal injections of anti-VEGF or steroids.
Laser treatment may be used to seal the leaking blood vessels and to scar the abnormal new vessels. While most people see some improvement in their vision, some people won’t have any improvement.
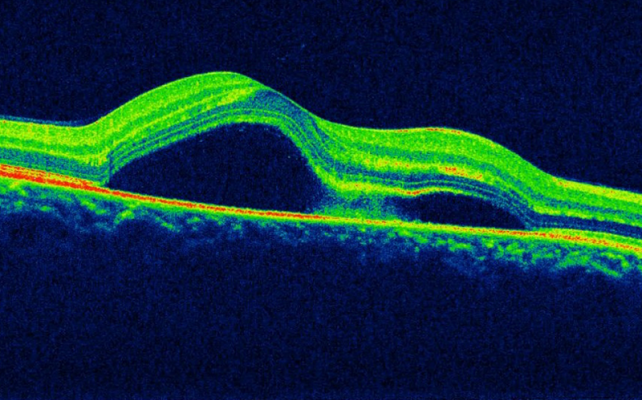
Floaters and Flashes
Floaters look like small hair-like or mosquito-like or cobwebs in the field of vision, especially when looking at something plain and light coloured (like a blank wall or a blue sky). While they seem to be in front of the eye, they are actually floating inside the eye.
Flashes can look like flickering lights or lightning streaks in the field of vision mostly seen at night or in dark rooms. They might be seen on and off for weeks, or even months.
As we age, the jelly inside the eye (called vitreous) starts to shrink. This process can create some clumps or strands of various shapes in the vitreous which cast a shadow on the retina and appear as floaters.
The vitreous then starts to pull away from the back of the eye, in a process called posterior vitreous detachment (PVD). Flashes are seen when the vitreous pulls on the retina. If the pull is strong, then the retinal blood vessels may rupture causing bleeding inside the eye. An even stronger pull can cause a retinal tear that can lead to retinal detachment and subsequent loss of vision.
Floaters are usually not serious, and they tend to fade or go away over time. Severe floaters can be removed by surgery, but this is seldom necessary. The risk of developing floaters in more in those with high minus numbers, after cataract surgery and in eyes that had swelling in the past.
It is important to show the eye doctor if:
- lot of new floaters are seen
- lot of flashes are seen
- a shadow appears in the peripheral (side) vision
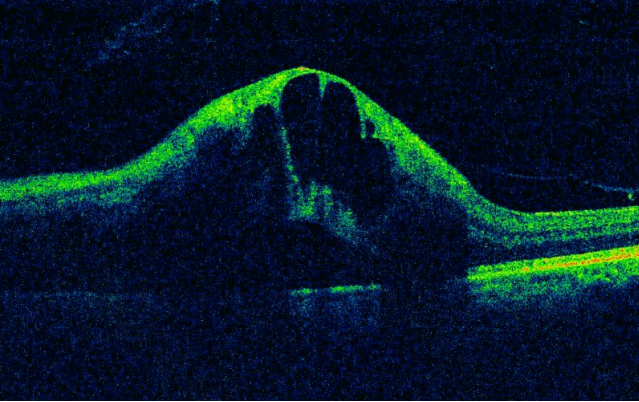
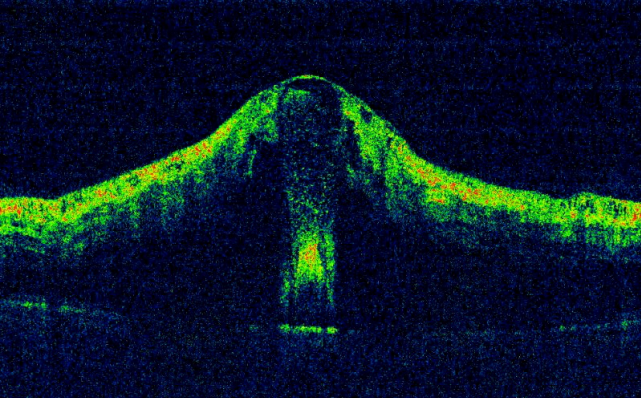
Macular Hole
Macula is the central, most vital part of the retina. Macular hole is when a tear or opening forms in the macula. As the hole forms, things in the central vision look blurry, wavy or distorted. As the hole grows, a dark or blind spot appears. A macular hole does not affect the peripheral (side) vision. As one gets older, the jelly of the eye (called the vitreous) begins to shrink and pull away from the retina. Sometimes this causes the macula to stretch and a hole to form. Sometimes it can also form when the macula swells from other eye disease or after an eye injury.
An OCT scan is done to obtain very detailed pictures of the macula. If the scan shows sufficient damage, then a surgery called vitrectomy is advised. In this surgery, the vitreous that is pulling on the macula is removed. An additional layer on the surface of the macula (called the ILM) that is less than a micron in thickness is also removed. A gas bubble is placed inside the eye to flatten the macular hole and hold it in place while the eye heals. The gas bubble slowly goes away on its own.
- One must keep the face down (avoid face up position at all times) for up to a week. This is to keep the gas bubble in place.
- One cannot fly in an airplane until the gas bubble is gone.
- If one needs to have any other type of surgery, be sure to tell the doctor before surgery that one has a gas bubble in the eye.
- The vision can improve after the macular hole closes. It may take several months for the hole to finish healing. How much vision one get back depends on the size of the macular hole and is not predictable. It also depends on how long the hole was there before one had surgery.
Like any surgery, this surgery also has some risks although extremely rare. They include eye infection, bleeding in the eye, detachment of the retina, increase in eye pressure and cataract.
Anti-VEGF injections
In certain diseases of the eye, a body chemical called VEGF (Vascular Endothelial Growth Factor) is released. This VEGF causes abnormal blood vessels to grow in the retina which tend to leak and affect the vision. Drugs that block the trouble-causing VEGF are called anti-VEGF drugs. These drugs slow down the growth of abnormal blood vessels in the eye. They are used to treat wet age-related macular degeneration (AMD), diabetic eye disease and other problems of the retina like a retinal vein occlusion. They are directly injected into the eye. Although it may be performed as an outpatient procedure, we prefer to inject it in the Operation Theatre to minimise the risk of infection.
Before the procedure, the eye is thoroughly cleaned and made numb with eye drops. A very thin needle (0.25mm) is passed through the white part of the eye and the drug is injected. Usually one does not see the needle itself. One may need to continue having these injections over many months. Some of the possible risks with these injections include eye infection (risk less than 1 in 1000 injections) and even lesser risk of detached retina and cataract formation.
For about 24 hours after injection, it is normal to feel like there is something in the eye, and to have mild eye pain with extra sensitivity to light. If these or any other side effects last longer, please contact your doctor right away. Eye redness or a bloody eye can last for a few days.
The commonly used anti-VEGF injections include Ranibizumab (Lucentis, Razumab), Bevacizumab (Avastin) and Aflibercept (Eylea).
Lucentis and Eylea are US FDA approved for intra-vitreal use and are on the more expensive side. Avastin, although not FDA approved for use in the eye, is used “off-label” for these conditions. This is primarily done to reduce the costs of multiple injections. Avastin is available in a larger vial meant for injecting into the blood vessels of the hand (intravenous use) for a completely different disease (colorectal cancer). But since the quantity needed for injecting in the eye is very less, the vial is shared amongst patients thus reducing the load of the costs for everyone. While the effectiveness of Avastin has been well proven, there have been slightly higher reports of eye infection or reactions noted with Avastin.
Retinal Lasers
Lasers are specialised narrow beams of light that have the ability to precisely focus on the target area. Due to the precise control they offer in the hands of the surgeon, they have been used for various purposes in medicine, especially in Ophthalmology.
There are various types of lasers and each laser has a different role to play in the treatment of eye diseases like cataract, glaucoma, retina, etc. In retina, mainly the Green lasers or the Red lasers are used. Depending on the purpose for which they are used in various retinal diseases. Laser procudures are not surgeries and are carried out in the out patient department only. After adequate dilatation, the patient is asked to sit or lie down (depending on the type of laser) and anesthetic drops are put in the eye. Laser shots are given at repeated intervals till the treatment is complete. There is usually no or mild pain. On occasion though some sensitive eyes could feel a stinging sensation in the eye or the head that is monmentary only.
There are no precautions to be taken either before or after the laser treatment.
Multiple such sittings may be needed based on the disease condition.
Pan Retinal Photocoagulation (PRP) laser: Diabetic Retinopathy, Retinal Venous Occlusions, Vasculitis, etc.
Barrage laser: Retinal degenerations, Retinal holes, Sub-clinical Retinal Detachments
Grid and Focal Laser: Diabetic Maculopathy
Photodynamic Therapy (PDT): Age-Related macular Degeneration, Idiopathic Polypoidal Choroidal Vasculopathy (IPCV)
ROP Lasers: Retinopathy of Prematurity
Central Serous Chorioretinopathy (CSCR /CSR)
In Central serous chorioretinopathy (CSCR), fluid accumulates under the
macula causing a swelling.
Normally there is an RPE (retinal pigment epithelial) pump in the retina that
prevents any fluid from accumulating. When the RPE pump does not work as
it should, fluid builds up under the RPE. As a result, a small elevation forms
under the retina, causing vision to become distorted.
CSCR usually affects one eye at a time.
Patients usually complain of distorted, dull or blurred vision. Some may see a dark round patch in the central vision and objects appear smaller or further away than they are.
Risk factors include:
- 30-50 year old Males
- Stress
- Sleep disturbances
- Smoking or tobacco intake
- Use of steroids in any form
- Type A behavior (aggressive and competitive behavior)
- High blood pressure
A retina specialist can diagnose CSCR just by examination. An OCT scan will tell the amount of fluid under the macula and decide the further course of action. A fluorescein angiography (FFA) identifies the point of leakage in case treatment is planned.
Most cases clear up in one or two months without any treatment. However if there is severe vision loss or the fluid does not go away, then laser treatment may be used. These treatments can seal the leak and restore vision.
In some cases, vision may not be as good as it was before the condition. About half of the patients are at risk of having it again. It is important to have regular follow-up exams because long-term fluid accumulation can lead to permanent vision loss.

Retinal Vein Occlusions (BRVO, CRVO)
The retina has one main artery and one main vein to carry blood to and fro. When the main retinal vein becomes blocked, it is called central retinal vein occlusion (CRVO). When branches (tributaries) of the retinal vein become blocked, it is called branch retinal vein occlusion (BRVO).
When the vein is blocked, blood and fluid spills out into the retina. The macula can swell from this fluid, affecting the central vision. Without blood circulation, nerve cells in the eye can die and more vision could be lost. At times body creates new blood vessels (neovascularisation) to compensate for the block. However these are fragile and create more problems. In BRVO these are usually found on the retina (NVE) or the disc (NVD) and can lead to bleeding in the vitreous. In CRVO they are formed on the iris (NVI) in front part of the eye causing eye pressures to rise (glaucoma).
Most patients present with blurry vision that happens suddenly or over several days. If bleeding occurs, it causes floaters or a sudden drop in vision. Glaucoma causes pain and pressure in the affected eye.
RVOs almost always happen in one eye at a time. RVO usually happens in people who are aged 50 and older. People with high blood pressure, diabetes, glaucoma and hardening of the arteries (called arteriosclerosis) are at a higher risk.
To lower your risk for BRVO, you should do the following:
- Eat a low-fat diet
- Get regular exercise
- Maintain an ideal weight
- Avoid smoking and tobacco
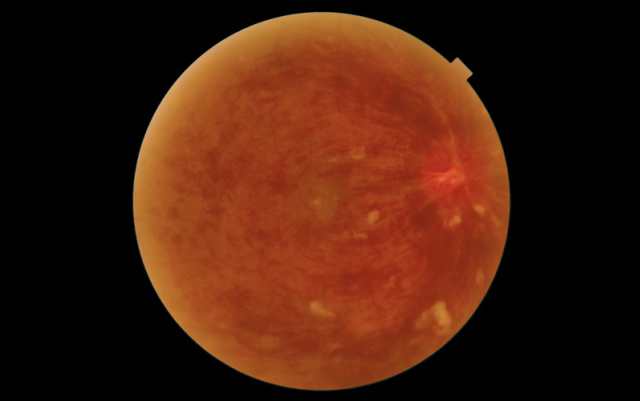
A retina specialist can diagnose an RVO by examination. An OCT scan will tell the amount of swelling on the macula and decide the treatment. A fluorescein angiography identifies the blocked vessels and also the abnormal new vessels.
Since BRVO cannot be cured, the main goal of treatment is to keep the vision stable. Swelling of the macula is best treated with intravitreal injections of anti-VEGF or steroids.
Laser treatment may be used to seal the leaking blood vessels and to scar the abnormal new vessels. While most people see some improvement in their vision, some people won’t have any improvement.
Floaters and Flashes
Floaters look like small hair-like or mosquito-like or cobwebs in the field of vision, especially when looking at something plain and light coloured (like a blank wall or a blue sky). While they seem to be in front of the eye, they are actually floating inside the eye.
Flashes can look like flickering lights or lightning streaks in the field of vision mostly seen at night or in dark rooms. They might be seen on and off for weeks, or even months.
As we age, the jelly inside the eye (called vitreous) starts to shrink. This process can create some clumps or strands of various shapes in the vitreous which cast a shadow on the retina and appear as floaters.
The vitreous then starts to pull away from the back of the eye, in a process called posterior vitreous detachment (PVD). Flashes are seen when the vitreous pulls on the retina. If the pull is strong, then the retinal blood vessels may rupture causing bleeding inside the eye. An even stronger pull can cause a retinal tear that can lead to retinal detachment and subsequent loss of vision.
Floaters are usually not serious, and they tend to fade or go away over time. Severe floaters can be removed by surgery, but this is seldom necessary. The risk of developing floaters in more in those with high minus numbers, after cataract surgery and in eyes that had swelling in the past.
It is important to show the eye doctor if:
- lot of new floaters are seen
- lot of flashes are seen
- a shadow appears in the peripheral (side) vision
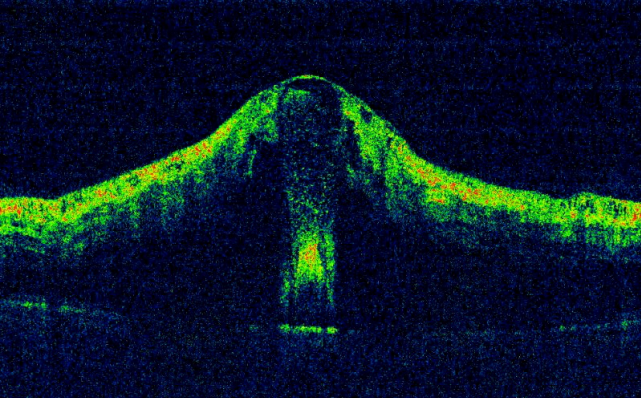
Macular Hole
Macula is the central, most vital part of the retina. Macular hole is when a tear or opening forms in the macula. As the hole forms, things in the central vision look blurry, wavy or distorted. As the hole grows, a dark or blind spot appears. A macular hole does not affect the peripheral (side) vision. As one gets older, the jelly of the eye (called the vitreous) begins to shrink and pull away from the retina. Sometimes this causes the macula to stretch and a hole to form. Sometimes it can also form when the macula swells from other eye disease or after an eye injury.
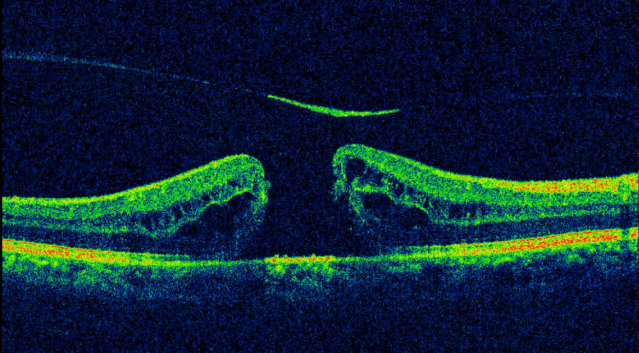
An OCT scan is done to obtain very detailed pictures of the macula. If the scan shows sufficient damage, then a surgery called vitrectomy is advised. In this surgery, the vitreous that is pulling on the macula is removed. An additional layer on the surface of the macula (called the ILM) that is less than a micron in thickness is also removed. A gas bubble is placed inside the eye to flatten the macular hole and hold it in place while the eye heals. The gas bubble slowly goes away on its own.
- One must keep the face down (avoid face up position at all times) for up to a week. This is to keep the gas bubble in place.
- One cannot fly in an airplane until the gas bubble is gone.
- If one needs to have any other type of surgery, be sure to tell the doctor before surgery that one has a gas bubble in the eye.
- The vision can improve after the macular hole closes. It may take several months for the hole to finish healing. How much vision one get back depends on the size of the macular hole and is not predictable. It also depends on how long the hole was there before one had surgery.
Like any surgery, this surgery also has some risks although extremely rare. They include eye infection, bleeding in the eye, detachment of the retina, increase in eye pressure and cataract.
Anti-VEGF injections
In certain diseases of the eye, a body chemical called VEGF (Vascular Endothelial Growth Factor) is released. This VEGF causes abnormal blood vessels to grow in the retina which tend to leak and affect the vision. Drugs that block the trouble-causing VEGF are called anti-VEGF drugs. These drugs slow down the growth of abnormal blood vessels in the eye. They are used to treat wet age-related macular degeneration (AMD), diabetic eye disease and other problems of the retina like a retinal vein occlusion. They are directly injected into the eye. Although it may be performed as an outpatient procedure, we prefer to inject it in the Operation Theatre to minimise the risk of infection.
Before the procedure, the eye is thoroughly cleaned and made numb with eye drops. A very thin needle (0.25mm) is passed through the white part of the eye and the drug is injected. Usually one does not see the needle itself. One may need to continue having these injections over many months. Some of the possible risks with these injections include eye infection (risk less than 1 in 1000 injections) and even lesser risk of detached retina and cataract formation.
For about 24 hours after injection, it is normal to feel like there is something in the eye, and to have mild eye pain with extra sensitivity to light. If these or any other side effects last longer, please contact your doctor right away. Eye redness or a bloody eye can last for a few days.
The commonly used anti-VEGF injections include Ranibizumab (Lucentis, Razumab), Bevacizumab (Avastin) and Aflibercept (Eylea).
Lucentis and Eylea are US FDA approved for intra-vitreal use and are on the more expensive side. Avastin, although not FDA approved for use in the eye, is used “off-label” for these conditions. This is primarily done to reduce the costs of multiple injections. Avastin is available in a larger vial meant for injecting into the blood vessels of the hand (intravenous use) for a completely different disease (colorectal cancer). But since the quantity needed for injecting in the eye is very less, the vial is shared amongst patients thus reducing the load of the costs for everyone. While the effectiveness of Avastin has been well proven, there have been slightly higher reports of eye infection or reactions noted with Avastin.
Testimonials
Hello..this is Mr Sameer Bhambere from thane. One month back my mom underwent the cataract operation for both her eyes within the span of 2 months. Done by Dr Nikhil Negular along with his efficient n prompt team. The experience was amazing n soothing for my mom. Her reaction was that I didn't even come to know when it started n ended. Dr nikhil took me in encrossed me in some talks by asking questions n was doing something thinking that he is preparing for the operation she too kept chatting but in 10 minutes he told my mom maushi zhale and she was amazed. A very spectaculared n well handled it was for us as with senior citizens operation word is tuff to be handled, but he made it ease for her. Overall a well equipped, clean, efficient set up lead by Dr Nikhil Negular and will go a long way. The knowledge of new technologies and standards carried him make an impact thus creating further faith with his down to earth n spectacular personality. I and my parents are really thankful to him and his entire staff for giving us a friendly n comfortable support and making life n vision simplier, easier and clearer for my mom.
Sameer Bhambere
Well what can I say. Dr. Dilip and Dr Aruna have been our Family eyecare Doctor. He has treated my father my mother me and my wife Thanks to his care I still am having good eyesight and have successfully kept cataract at bay. My parents have been successfully operated by him and never had to face any issues thereafter. Great Doctor Great team just everything about Bhaskar eye care is about Caring.
Hariharan Iyer
Hi . My husband Suhas had his cataract surgery at Bhaskar eye care . Apart from the medical proficiency of Dr Dilip Gaitonde , we were extremely impressed by the overall care and efficiency.....the very courteous and helpful staff , the cleanliness around , the soothing soft music in the room , the personal attention of Dr. Dilip and his anasthetist wife , Dr Aruna ....instantly allayed whatever apprehentions we had . All this matched the post - operative care and follow up. An almost holistic experience......!
Almitra Shah
I had cataract surgery for both eyes recently at Bhaskar eye care on Ghodbhunder road. Dr Nikhil Negalur and his team were very polite, supportive and caring. I was very impressed by their willingness to answer all my questions. Dr Nikhil took the time to call me after the surgery to see how I was doing - I sincerely appreciate this personal attention. Even during the surgery he made sure that I was comfortable. Ms Vaibhavi was also very kind and patient in clarifying doubts. Right from the people at the reception desk, to the doctors and even the service staff, all the people here provide the best care possible. I wish them success in all they do and may they scale greater heights.
Lakshmi Iyer


